Balloon-occluded retrograde transvenous obliteration (BRTO)
What is BRTO?
Portal hypertension refers to high blood pressure in the liver. One of the major possible complications of portal hypertension is gastric variceal bleeding. Varices are dilated vessels which may rupture, causing variceal bleeding. Gastric variceal bleeding describes the bleeding that occurs when dilated vessels in the stomach rupture, and is associated with high morbidity and mortality rates.
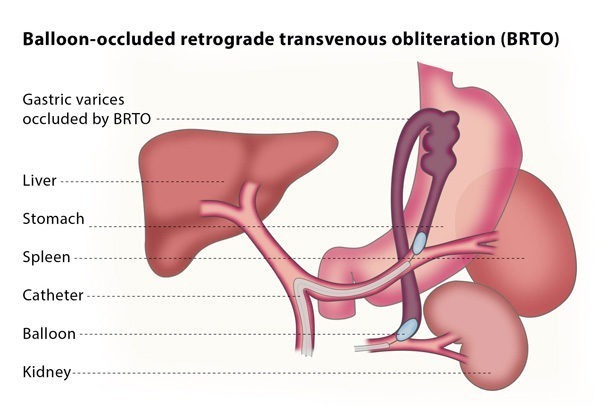
BRTO is a minimally invasive technique that is used to treat gastric variceal bleeding. The procedure involves blocking the dilated vessels, reducing the risk of rupture. It can be used in addition to or as an alternative to TIPS, which is the primary treatment for gastric varices. TIPS aims to relieve the pressure on the dilated vessels by creating new connections between blood vessels in the liver using a shunt.
How does the procedure work?
The interventional radiologist will insert a balloon catheter (a thin, flexible tube with a tiny balloon at one end) through a vein in your thigh or neck and guide the catheter to the liver using fluoroscopy for guidance. The catheter is then directed to the gastrorenal or gastrocaval shunt and the balloon is expanded to block the shunt.
The interventional radiologist will then perform a venography, which is a type of imaging technique in which X-rays are used to see the vessels clearly. This will allow the interventional radiologist to confirm exactly which vessels need to be treated and if there are any other abnormal or dilated vessels which have not previously been identified. A medication will then be injected into the dilated vessels through the catheter, until they are completely filled. This medication will remain in the vessel for a short period of time, and will then be removed under fluoroscopy.
Another venography will then be performed, to confirm that the blood flow in the shunt has stopped. Finally, the balloon will be deflated and the interventional radiologist will withdraw the catheter.
Why perform it?
You may be advised to undergo this procedure if you are at risk of or already have gastric variceal bleeding and hepatic encephalopathy as well as a gastrorenal shunt. Hepatic encephalopathy refers to the worsening of brain function that is caused by a damaged liver.
Although TIPS has been considered the standard therapy for gastric varices that have been unresponsive to other treatments, recent reports have stated that BTRO is a less invasive and more effective way to manage varices than shunt surgery or TIPS. TIPS does not always cause the disappearance of gastric varices, while BRTO can in most cases completely destroy these vessels.
BRTO has tended to be used to prevent gastric variceal bleeding. It is also an effective therapy for sclerosis (narrowing) of new portosystemic shunts with the additional complication of hepatic encephalopathy. One of the greatest advantages of BRTO is its preservation of liver function. Moreover, the increase of blood flow in BRTO can also improve liver function in cases where the patient has cirrhosis (scarring of the liver).
A further possible reason to have an angiography is as a pre-operative procedure, meaning your doctor would like a more detailed knowledge of your anatomy. This knowledge is beneficial for procedures such as revascularisation (restoring blood to an area with a restricted blood supply), local tumour resection (surgically removing a tumour) and organ transplantation.
A diagnostic angiography also aids with diagnosis and treatment of post-operative or traumatic complications. It can also be used during procedures such as thrombolysis, angioplasty, stenting and embolization as it gives the interventional radiologist performing the procedure a clearer view of what they are doing.
What are the risks?
Procedure-related complications are minor and include bleeding and infection. In rare cases, the blockage of the blood to the gastric varices can further increase the pressure on the liver, causing damage to the liver.
The most serious complications of the procedure, however, are related to the medication used to block the vessels, which is called ethanolamine oleate. Inflow of a relatively large amount of ethanolamine oleate can lead to serious complications. These complications include pulmonary embolism (blockage in a lung’s main artery), fluid in or around the lungs, hypersensitivity, fever, problems with blood flow to the heart and the formation of small blood clots in vessels throughout the body. Ethanolamine oleate also causes haemolysis, which is the rupturing of red blood cells. To prevent this from occurring, only a low dose of the medication is used.