Bronchial stenting
What is tracheobronchial stenting?
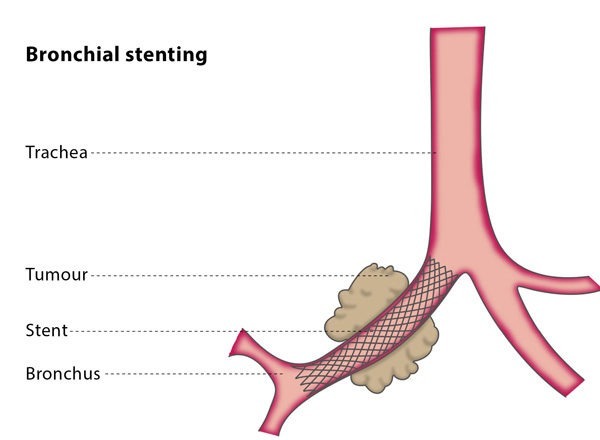
Your airway system consists of the trachea, which is then divided into different sections, called the main stem and segmental bronchi, which supply both your lungs. Diseases which block the airways are very dangerous, as they may cause the lungs to collapse and prevent the patient from inhaling enough air, causing death.
A stent is a metal mesh tube that is inserted over a guidewire and placed in a vessel in order to keep it clear. Tracheobronchial stenting refers to the placing of a stent in a patient’s airways to treat or prevent restricted airflow. The procedure is minimally invasive and is most often used to relieve symptoms caused by cancerous tumours blocking airways.
How does the procedure work?
You will have a general anaesthetic for the procedure, which will be carried out in an operating theatre by a team of interventional radiologists and surgeons. The doctors will use fluoroscopy and a bronchoscope (a tiny camera inserted into your body on a tube) for guidance.
An interventional radiologist will thread a guidewire into your airway system so that the stent can be guided to the correct location. Once placed in the affected area, the stent will expand, clearing the airway.
An oncologist may take a tissue sample before the stent is placed, if this would be beneficial in planning your optimal treatment.
In most cases, patients stay in hospital overnight, and you will be discharged from hospital once you have had a consultation with the thoracic and oncology teams who will provide your follow-up care.
Why perform it?
If you have a cancerous growth in your trachea or bronchi which cannot be operated on and is affecting your breathing, having a stent placed may relieve your breathlessness while you undergo chemotherapy and/or radiotherapy.
In some cases, a stent is placed to treat fistulas (holes) that have developed in the airway system or to treat blockages in the airway that are not cancerous. If the patient is a child, the use of biodegradable stents, which are absorbed over time, is recommended
What are the risks?
The majority of cases (over 95%) are successful, and most patients (70-80%) see significant clinical improvement 24-48 hours after the procedure. In 10-20% of cases, the stent migrates, meaning it moves to another part of the body. If this occurs, the stent will be removed and replaced with a new stent.
Other possible complications include bleeding, chest infection, temporary chest pain and the risk of the airways reacting to the stents, which can cause spasm and breathlessness.