Endovascular treatment of abdominal aortic aneurysms (EVAR)
What is endovascular aortic repair (EVAR)?
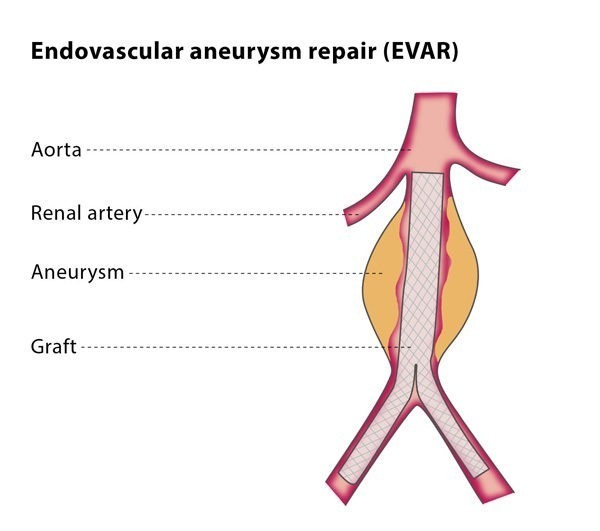
The aorta is the largest vessel in your body and carries the blood from your heart to the rest of your organs. An aneurysm occurs if the arterial wall weakens and develops a bulge like a balloon into which blood flows, further increasing the pressure on the weakened wall. Abdominal aortic aneurysms (AAA) are also known as ‘the silent killer’ because once they grow and rupture, there is an 80-90% risk of immediate death.
EVAR is a minimally invasive procedure in which an interventional radiologist places a covered stent (a metal mesh tube covered with fabric) into the aorta so that blood can flow through normally but does not flow to the weakened wall, which is no longer exposed to high pressure, preventing it from bursting. The stent is inserted through an artery in the patient’s groin, using X-rays to guide the stent to the aneurysm.
How does it work?
You will be given a combination of an epidural, local anaesthetic, or general anaesthetic for the procedure. The interventional radiologist will make a small cut at the top of each leg so that they can insert a short tube (known as a sheath) into the artery, through which all the other required devices are placed. Using fluoroscopy (live X-Rays) for guidance, the interventional radiologist will insert guidewires and catheters (thin flexible tubes) into the aorta. A contrast medium (dye) will be injected into the area being treated so the exact location of the aneurysm and other important branches of the aorta can be seen under imaging. The interventional radiologist will then use the guidewire to advance a stent to the aneurysm.
When the stent is placed in the correct location, it will expand, sealing the aneurysm and restoring normal blood flow through the vessel.
After the procedure, your vital signs will be monitored and you will stay in hospital for 1-2 days. You may experience bruising and pain, though this can be treated with standard painkillers. Moving around is encouraged once you are able to do so. You will need to have the stent regularly checked using CT or ultrasound to ensure that it is in good condition and to avoid long-term problems.
Why perform it?
If you have a small AAA that has a diameter of less than 5.5 cm, it is less likely to rupture, so it is recommended that the aneurysm is regularly monitored by a vascular expert. If, however, you have an aneurysm that is smaller than 5 cm but it is growing by more than 1 cm every year or it is causing symptoms such as back pain and tenderness, EVAR may be beneficial for you.
If your aneurysm is larger than 5.5 cm, you will need treatment to prevent the aneurysm from rupturing. EVAR is a possible treatment option.
What are the risks?
EVAR is recommended as a preventative treatment to avoid aneurysm rupture and death. The majority of patients suffer no immediate major problems and rupture of the aneurysm is avoided in over 99% of patients. There are lower rates of pain and serious complications than with surgery, but the main limitations of EVAR are that the stent may move slightly and that blood may start collecting in the aneurysm again. This means that you will require regular monitoring, so that if any problems do occur they can be identified and fixed as soon as possible.
Minor complications include the risk of bruising and infection. There are some serious complications associated with the procedure, including death, stroke, tissue death, limb loss and injury to the kidneys. The rate of serious complications is estimated to be less than 15%, and the risk of death during the procedure is less than 1.5%, which is nearly three times lower than the risk of dying during open surgery (around 4.5%). Some patients react to the iodine in the dye used for imaging, which can affect the kidneys.