Gastrojejunostomy
What is a gastrojejunostomy?
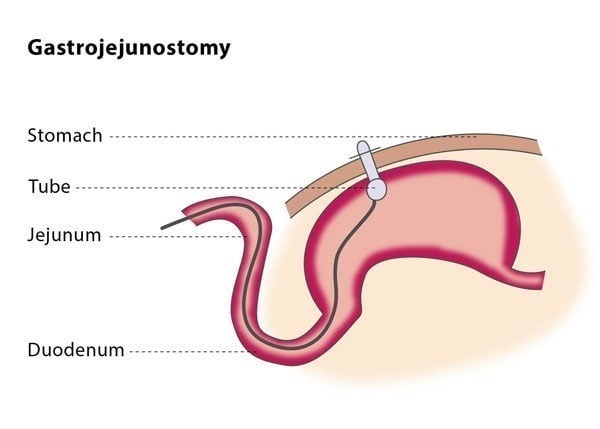
A gastrojejunostomy is a minimally invasive procedure in which a feeding tube (called a gastrojejunostomy tube or GJ tube) is inserted through the stomach and into the small intestine. This allows nutrition to be given directly into the jejunum, bypassing the mouth, throat and stomach.
The GJ tube provides nutritional support to patients who are unable to eat and are unsuitable for a gastrostomy tube due to a blockage preventing food from passing from the stomach into the small intestine, severe paralysis of part of the stomach or a high risk of choking.
How does the procedure work?
If you are on any medication which prevents blood clotting, you will stop taking it before the procedure, if possible.
You should not eat anything before the procedure. The interventional radiologist will insert a tube in your nose which will go into your stomach (called a nasogastric tube) and then will perform an ultrasound of your stomach to check the position of your liver and confirm that the tube is correctly placed.
The procedure is usually performed under local anaesthesia or moderate sedation. You may be given antibiotics to prevent infection, but this is not always necessary. You will lie on your back on the fluoroscopy table.
The procedure is similar to that of percutaneous gastrostomy. In most cases, you will be given a medication which temporarily paralyses the muscles in your stomach. The stomach puncture in gastrojejunostomy is aimed at the area where your stomach connects with your small intestine as this is where the tube will go.
The interventional radiologist will then insert a catheter along with a guidewire into the jejunum, which is the middle section of your small intestine. The interventional radiologist will use dilators to expand the skin opening and then insert the GJ tube. To check the proper positioning of GJ tube,the interventional radiologist will inject a small amount of contrast media (dye) through the tube so that the position of the tube tip can be confirmed using X-ray.
You will probably be required to stay in hospital overnight, although a gastrojejunostomy can also be performed as an out-patient procedure. You may experience slight discomfort at the entry point of the catheter for the first few hours following the procedure. The location of the tube will be checked daily for signs of leakage or infection. You will be allowed to eat between 8-24 hours after the gastrojejunostomy, after you have consumed 50 ml of water per hour for at least four hours without any negative effects. The T-fasteners used in the procedure can be safely removed 10-14 days after the procedure.
Why perform it?
The indications that a gastrojejunostomy may be beneficial for you are similar to those for a gastrostomy – you may be advised to have this procedure if you are unable to eat normally. The most common reasons for this are neurological causes (such as stroke or dementia), anatomical situations (such as during correction procedures of cleft lip and palate anomalies) and if a blockage is preventing food passing from your stomach to your small intestine.
Patients with gastro-oesophageal reflux may benefit from GJ feeding as the feed is delivered directly to the jejunum rather than the stomach. This stops stomach contents travelling back (reflux) up the oesophagus (food pipe), causing pain and potentially chest infection if the liquid is inhaled into the lungs (aspiration).
If the interventional radiologist cannot access your stomach for the gastrostomy tube placement or you have previously had a gastrectomy (the surgical removal of all or part of your stomach), they may directly puncture your jejunum (the middle part of your small intestine) instead – this is known as a jejunostomy.
The reasons why this procedure may not be suitable for you are also similar to those for a gastrostomy. You should not undergo the procedure if you have a blood-clotting disorder, if your colon or liver is positioned between your stomach and abdominal wall (as this prevents a safe access route), if you have peritonitis (inflammation of the thin tissue wall which covers most of your abdominal organs as well as the inner abdominal wall), or if you suffer from untreatable massive ascites (abnormal fluid in your abdomen).
This procedure may not be suitable for you if you have dilated blood vessels in your gullet or stomach, changes in the top layer of the stomach lining, if you have abnormal cell growth in the wall of your stomach, cancer that affects the lining of the abdominal cavity, if you are morbidly obese or if you have had previously had surgery in the area.
The technical success rate ranges from 85-95%.
What are the risks?
The possible complications for a gastrojejunostomy are similar to those for a gastrostomy procedure: peritonitis (inflammation of the thin tissue wall within your abdomen), skin infection around the catheter entry site and bruising, as well as injury to the colon.
Some patients develop a condition called intussusception, when part of the intestine folds onto another section of the intestine, causing bowel obstruction